Embryo grading and its importance: Embryology Training in India
Medline Academics offers structured embryology training in India that bridge classroom knowledge with real-world ART practice. Every course is designed to impart hands-on experience, scientific reasoning, and the confidence to work in a functioning IVF lab environment.
Embryo grading means assigning a grade to the embryos. Be it your day 2, day 3 or blastocyst grade, all these embryos need to have a particular grade. You can't every time be saying cell numbers, fragmentation, amount of disturbance in the embryo. Instead, we should grade them as A, B, C or D. There are some grading systems which use a numerical form as 1, 2, 3, 4. You can pick either, but embryo grading is an extremely critical part of your embryology process. A lot of embryologists may differ.
They may feel that ICSI or other things like OPU or denudation are important. I'm in no way saying that they are not. But embryo grading will help you elevate your success and the pregnancy rates to a different level. The reason is that if you are able to pick the best embryo out of a cohort, that easily will be the best embryo that you are transferring to your patients. So, embryo grading is extremely important. There are many forms of embryo grading available - Ranging from the Gardner system to ACEBIR. ACEBIR – is extremely detailed.
· For embryologists - it is really important that you train all the embryologists working in your lab with a particular grading system and standardize it.
· For Patients - please ask your lab about what grade of embryos were transferred. Because that will make or break your cycle.
So, you need to know not just the quantity of embryos that were used in your cycle, but also the grading. So, next time you visit your clinic, please ask them what were the grades of embryo transferred. And that will help answer a lot of your queries.
Dr. Kamini Rao Hospitals – an IVF Hospital in Bangalore, embryologists are trained with a standardized grading system to ensure uniform interpretation in the lab. The success of an entire IVF cycle is dependent on the precision with which an embryo is selected. In this hospital, every stage - Day 2, Day 3 cleavage stage or Day 5-7 blastocysts, is carefully documented and graded. The aim behind doing this is not just to identify embryos, but to select the embryo with the highest chance of implantation and live birth.
Can you pick an embryo that is most likely to produce a live birth simply by looking at it under the microscope?
Sounds like an easy question to answer but the reality is far more complex.
· First, they culture embryos to the blastocyst stage. This usually takes 5-7 days.
· Second, embryos that reach the blastocyst stage are frozen so they can be placed in the uterus at a more optimal time.
· Third, chromosome testing of the embryos known as PGT is performed for women over the age of 35.
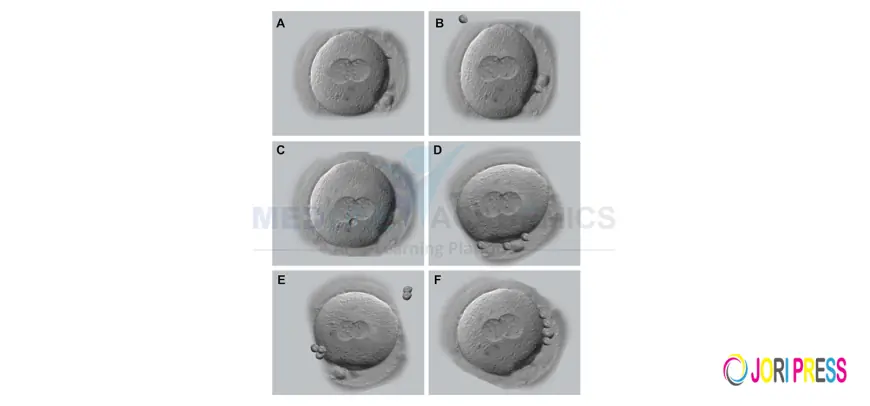
How are blastocyst graded?
Across the planet there are many different grading systems. This becomes a problem because a scientific study published using one system isn't necessarily going to have the same results as another system. In general, however, blastocyst grading looks at three different things.
· First is the size of the blastocyst.
A developing blastocyst fills with fluid in the middle. This causes the blastocyst to grow larger like a water balloon. We call this expansion. A blastocyst that is more expanded isn't necessarily a better-quality blastocyst but it does make it easier to see different cells developing in the embryo.
· The second criteria look at a group of cells known as the inner cell mass. These are the cells that go on to form the foetus.
· The third criteria look at the remainder of the cells. These cells are called the trophoblast. These cells eventually developed into non-fetal tissues like the placenta.
There are many problems that we run into with blastocyst grading.
· The first problem is timing. The microscopic appearance of the blastocyst can change even over the course of a few hours. What looks poor at one moment may look better at another time.
· The second problem is called intra-observer variability. This means that two well-trained embryologists can look at the same embryo at the same time and give it a different grade. Remember that these assessments are very subjective and sometimes the differences can be very subtle.
· A third problem is that grading systems may not be predictive of whether a live birth occurs. In fact, if you review studies that have looked at grading blastocysts, you will find that they have reached different conclusions.
For example, some studies found that the grade of the inner cell mass predicted pregnancy potential. Other studies found that the inner cell mass didn't matter but that the grade of the trophoblast was important. These different factors aren't always similar.
It is possible to have a blastocyst with a pretty inner cell mass and a not-so-pretty trophoblast or just the reverse. Which one should be prioritized?
Unfortunately, there is no universal agreement on this. Is all this confusing enough yet? Just wait. It gets worse. We know that many of the embryos that have chromosome abnormalities will never develop to the blastocyst stage. This is one of the reasons that doing blastocyst embryo transfers is a good idea. Blastocysts are less likely to have chromosome abnormalities compared to earlier stage embryos. But some of them still will. In fact, some really beautiful blastocyst embryos can have chromosome abnormalities. Studies show that transferring chromosomally abnormal blastocysts have an extremely poor chance of becoming a live birth.
What if you have an embryo that reached the blastocyst stage and looked good enough to biopsy so you could test the chromosomes and the results were normal? Does the grade even matter at that point? Maybe not. A few studies have looked at this. Some have found no impact of the grade. Some others have but again, they don't always agree on which criteria are important to look at.
You may have heard that there are embryo incubators that have cameras in them that can take pictures of the embryo every few minutes as it is developing. These are called time-lapse incubators. Instead of looking at the embryo at just one point, you can look at it at hundreds of time points and do all sorts of calculations like how long does it take the embryo to divide from two cells to four cells. Does this sort of embryo grading help to select the most viable embryos? At this point, there is no proof that these systems are any better for selecting the embryos with the best potential for a live birth. Many IVF centres are producing studies using these time-lapse incubators so there is hope that in the future, we may find that these systems can do more than just produce cool videos.
Another technology we are looking at for the future of embryo selection is artificial intelligence.
Most IVF labs will freeze or biopsy only what they feel are good quality blastocysts. Beyond that, the role of embryo grading in determining which embryo will produce a live birth is really uncertain and varies significantly from one lab to another and even from one embryologist to another. IVF is stressful enough. Try not to get too fixated on embryo grading. Some great looking embryos may still fail to produce a live birth and some not-so-great looking embryos still might.
Interested to transform your learning into practice?
Medline Academics offers structured embryology training in India that bridge classroom knowledge with real-world ART practice. Every course is designed to impart hands-on experience, scientific reasoning, and the confidence to work in a functioning IVF lab environment. Techniques like ICSI, oocyte retrieval or denudation are important, but the difference between an average outcome and an exceptional one often lies in how accurately embryos are graded, selected and handled within the embryology lab. Medline Academics Fellowship in Embryology introduces students to AI-based embryo selection concepts, Time-lapse monitoring systems, PGT workflows in advanced cases and Clinical decision-making for high-risk patients. Because a good embryologist is not only technically skilled, they are
Responsible
Ethical &
Patient-centric!
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0