Leg Infection in Diabetics: Understanding Arterial Leg Ulcers and Diabetic Foot Infections!
Leg infections, arterial leg ulcers, and diabetic foot infections represent severe complications of diabetes that require prompt and effective management.
Diabetes is a chronic disease that affects millions of people worldwide, often leading to severe complications if not managed properly. Among these complications, leg infections, arterial leg ulcers, and diabetic foot infections are particularly concerning. These conditions not only impair quality of life but can also result in severe morbidity, including amputation, if not treated promptly and effectively. This article delves into the nature, causes, and management of these diabetic complications.
Leg Infection in Diabetics
Diabetes impairs the body's ability to heal and fight infections due to high blood sugar levels, which can weaken the immune system. This makes diabetes patients more susceptible to infections, particularly in the lower extremities. Neuropathy (nerve damage) and poor circulation contribute to this increased risk. Neuropathy can cause loss of sensation in the feet, preventing individuals from noticing injuries or ulcers until they become infected. Poor circulation, often due to peripheral artery disease (PAD), reduces blood flow to the legs, further complicating healing processes.
Arterial Leg Ulcers
Arterial leg ulcers, also known as ischemic ulcers, occur due to inadequate blood flow to the lower extremities, primarily caused by PAD. PAD is prevalent among people with diabetes due to the association of diabetes with atherosclerosis, a condition characterized by the hardening and narrowing of the arteries. Arterial ulcers are typically found on the toes, feet, or lower legs and are often painful.
Symptoms and Diagnosis
Symptoms: The ulcers appear as punched-out sores with well-defined borders and a pale or necrotic base. Other signs of poor circulation, such as cold skin, hair loss on the legs, and weak pulses in the feet, usually accompany them.
Diagnosis: Diagnosis involves a physical examination, assessment of the patient's medical history, and tests such as the ankle-brachial index (ABI) to measure blood flow. Imaging studies like Doppler ultrasound or angiography may be used to evaluate the extent of arterial blockages.
Management and Treatment of Leg Infection in Diabetic
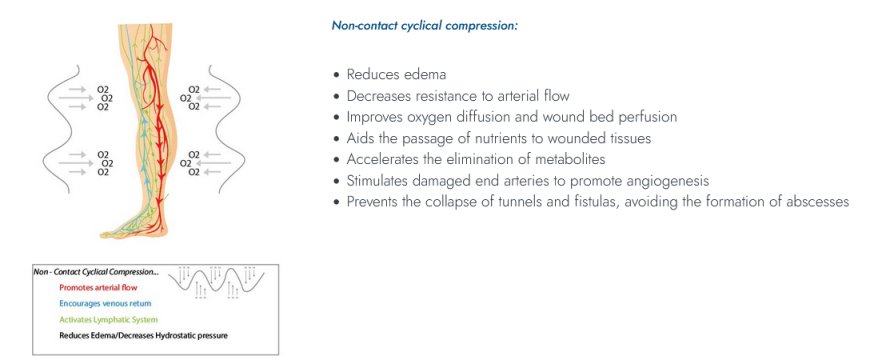
Medical Management: Treatment of leg infection in diabetic focuses on improving blood circulation and wound care. Medications may include anti platelet agents, cholesterol-lowering drugs, and pain relievers. In some cases, angioplasty or bypass surgery may be necessary to restore adequate blood flow.
Wound Care: Proper wound care involves cleaning the ulcer, removing dead tissue (debridement), and using appropriate dressings to promote healing and prevent infection. Patients are advised to avoid pressure on the affected leg and to keep the limb elevated to reduce swelling.
Diabetic Foot Infections
Diabetic foot infection is a significant concern due to their potential to progress rapidly and cause serious complications. These infections often start from minor cuts, blisters, or ulcers that become infected due to the impaired immune response in people with diabetes. Foot infections are classified based on severity, ranging from mild (limited to the skin and superficial tissues) to severe (involving deeper tissues, bones, or joints).
Symptoms and Diagnosis
Symptoms: Symptoms include redness, swelling, warmth, and pain in the affected area. Pus or discharge may be present, and fevers and chills can occur in severe cases.
Diagnosis: Diagnosis is based on clinical examination and, if needed, laboratory tests such as blood tests, cultures from the infected site and imaging studies like X-rays or MRIs to check for bone involvement.
Management and Treatment
Antibiotics: Antibiotic therapy is the cornerstone of treatment for diabetic foot infections. It is tailored based on the severity of the infection and the results of culture tests.
Surgical Intervention: In severe cases, surgical intervention may be required to drain abscesses, remove infected tissue, or amputate affected parts to prevent the spread of infection.
Wound Care and Prevention: Proper foot care is crucial for preventing infections. Patients are advised to inspect their feet daily, keep them clean and dry, wear proper footwear, and manage blood glucose levels effectively. Regular check-ups with a healthcare provider specializing in diabetic foot care are essential.
Conclusion
Leg infections, arterial leg ulcers, and diabetic foot infections represent severe complications of diabetes that require prompt and effective management. Through a combination of medical treatment, surgical intervention when necessary, and diligent self-care practices, individuals with diabetes can reduce their risk of these debilitating conditions. Early diagnosis and intervention are vital in preventing severe outcomes and maintaining a good quality of life for diabetic patients.
For more information about Diabetic foot infection, switch to Advanced Oxygen Therapy Inc. for the best wound care or healing programs.